Pune, July 24, 2024 (GLOBE NEWSWIRE) -- U.S. Pharmacy Benefit Management Market Size Analysis:
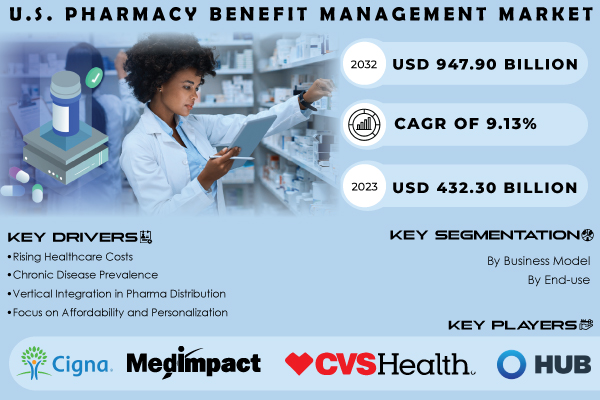
“According to SNS Insider Research, The U.S. Pharmacy Benefit Management Market was valued at USD 432.30 billion in 2023, and is anticipated to reach USD 947.90 billion by 2032, and grow at a CAGR of 9.13% over the forecast period 2024-2032.”
Pharmacy Benefits Managers are basically mediators who run the prescription drug programs for several health insurance companies in the US. These include employer-paid plans, Medicare Part D and government programs. The key functions of pharmacists are outlined by the American Pharmacists Association as PBMs play a role of gatekeepers to drugs by managing the formulary, which is essentially a list of approved medications within an insurance plan. This has direct effects on the drugs that can be affordable and reached by all patients and they use the leverage generated by higher volumes and bargaining to negotiate discounts from drug companies, which in turn serve as a break on growth in costs of prescription drugs for health plans and patients. Not only they create and maintain networks of pharmacies, but deal with pharmacy dispensing as simply another area for the patient to receive their medication. And, perhaps most importantly to pharmacies, PBMs process and pay claims from providers so that reimbursement for their services is virtually guaranteed on time.
Pharmacy Benefit Managers are the middlemen they exert significant power at multiple key stages like PBMs generate and manage lists of covered drugs means formularies for insurers. These lists determine which drugs are easily accessible and affordable to patients - a crucial determinant of what treatment options someone has as well as how much they must pay out-of-pocket. PBMs use their purchasing power that is organized on behalf of many health plans. This enables them to bargain for rebates and discounts with drug manufacturers, in the hope of overall lowering costs through the supply chain on their medications. They create and supervise the pharmacy networks that PBMs provider management module require. This guarantees patients easy access to pharmacies that carry the particular drugs covered in their health plans.
Get a Sample Report of U.S. Pharmacy Benefit Management Market@ https://www.snsinsider.com/sample-request/4407
Major Players Analysis Listed in this Report are:
- MedImpact
- Elixir Rx Solutions LLC
- CVS Health
- HUB International Limited
- Cigna
- Anthem
- Prime Therapeutics LLC
- Change Healthcare
- CVS Caremark
- Express Scripts
- OptumRx
- Other Players
According to a recent report released by the Federal Trade Commission in July 2024, this is just part of an alarming trend in the pharmacy benefit management market that only six companies own 96% of the pharmacy benefit management market and manage approximately 95% of total U.S. prescriptions filled share. In other words, a handful of companies play an incredibly significant role in terms of how hundreds upon millions of Americans are able to get their health care service.
U.S. Pharmacy Benefit Management Market Report Scope:
| Report Attributes | Details |
| Market Size in 2023 | US$ 432.30 Billion |
| Market Size by 2032 | US$ 947.90 Billion |
| CAGR | CAGR of 9.13% From 2024 to 2032 |
| Base Year | 2023 |
| Forecast Period | 2024-2032 |
| Historical Data | 2020-2022 |
| Key Growth Drivers | •Rising Healthcare Costs • Chronic Disease Prevalence • Vertical Integration in Pharma Distribution • Focus on Affordability and Personalization |
Do you have any specific queries or need any customization research on U.S. Pharmacy Benefit Management Market, Enquire Now@ https://www.snsinsider.com/enquiry/4407
U.S. Pharmacy Benefit Management Market Driven By Increased Accessibility And Digital Integration
- Expanding Medication Accessibility
- Growth in Patient Population
- Enhanced Negotiation Power
U.S. Pharmacy Benefit Management Market Opportunities: A Digital Revolution in Healthcare Management
- Patient Engagement
- Real-Time Data
- Cost Control
- Digital Treatment Programs
- Chronic Disease Management
- PBMs as Optimization Experts
Only 6 Players Of The U.S. Pharmacy Benefit Management Market Holds 96% Market Share
The U.S. pharmacy benefit management (PBM) landscape is highly concentrated, per data platform Statista. Its share is most leading by three companies:
- CVS Caremark: Leading the pack with 33% market share.
- Express Scripts: Following closely with 24% market share.
- OptumRx: capturing a significant 22% market share.
U.S. Pharmacy Benefit Management Market Key Segmentation:
By Business Model
- Standalone PBM
- Health Insurance Providers
- Retail Pharmacy
By End-use
- Commercial
- Federal
Together, these three giants leading 79% of the pharmacy benefit management market in America. Other players are a relative noteworthy: following the top three, Humana Pharmacy Solutions 8%, Prime Therapeutics-5% and MedImpact Healthcare Systems take up only 4% of the pharmacy benefit management marketplace - in total.
Buy a Complete Report PDF of U.S. Pharmacy Benefit Management Market Analysis & Industry Outlook 2024-2032@ https://www.snsinsider.com/checkout/4407
Recent Advancement Announced By One Of The Leading Player On Its Way In Future
Optum Rx is beginning a new pharmacy benefits option called the OptumRx Clear Trend Guarantee. To tackle one of the biggest challenges in healthcare, this ground-breaking model delivers a firm price per member based upon drug costs across pharmacy such as retail, home delivery and specialty drugs. Its main goal is to budgeting and controlling costs easier for plan sponsors which may lower the costs for families & individual. Scheduled for 2025, this offering is part of a suite of clear pricing solutions available from Optum Rx.
Table of Contents – Major Key Points
1. Introduction
2. Industry Flowchart
3. Research Methodology
4. Market Dynamics
5. Porter’s 5 Forces Model
6. Pest Analysis
7. U.S. Pharmacy Benefit Management Market Segmentation, By Business Model
8. U.S. Pharmacy Benefit Management Market Segmentation, By End-use
9. Company Profiles
10. Competitive Landscape
11. Use Case and Best Practices
12. Conclusion
Access Complete Report Details of U.S. Pharmacy Benefit Management Market Analysis 2024-2032@ https://www.snsinsider.com/reports/u-s.-pharmacy-benefit-management-market-4407
[For more information or need any customization research mail us at info@snsinsider.com]
About Us:
SNS Insider is one of the leading market research and consulting agencies that dominates the market research industry globally. Our company's aim is to give clients the knowledge they require in order to function in changing circumstances. In order to give you current, accurate market data, consumer insights, and opinions so that you can make decisions with confidence, we employ a variety of techniques, including surveys, video talks, and focus groups around the world.
