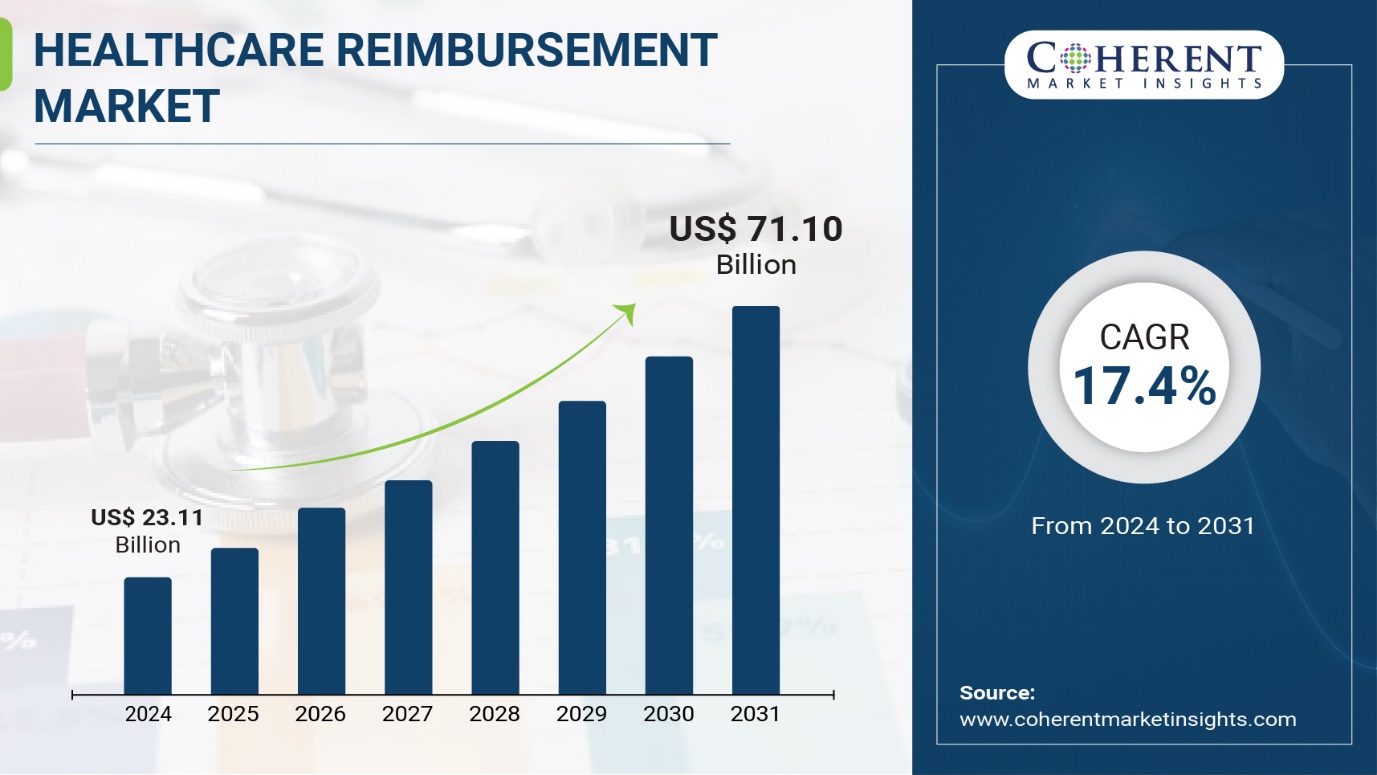
Burlingame, Aug. 14, 2024 (GLOBE NEWSWIRE) -- Coherent Market Insights published a report, titled, "Healthcare Reimbursement Market, By Claim (Fully paid and Underpaid), By Payer (Private Payers and Public Payers), By Service Provider (Physician office, Hospitals & Clinics, Diagnostic Laboratories, Medical Equipment & Supplies, Others): Market Size And Share Analysis - Growth Trends And Forecasts, 2024-2031”. According to the report, the global healthcare reimbursement market was valued at $23.11 billion in 2024, and is estimated to reach $71.10 billion by 2031, growing at a CAGR of 17.4% from 2024 to 2031.
Request Sample Report: https://www.coherentmarketinsights.com/insight/request-sample/7108
Market Dynamics:
The healthcare reimbursement market is driven by the rising healthcare expenditure across the globe. Healthcare cost has been continuously increasing, which is putting pressure on the patients as well as insurer companies. As per data by World Health Organization, global healthcare spending is expected to increase from $7.8 trillion in 2020 to $10 trillion by 2030. This increasing healthcare spending is demanding need for more organized and automated healthcare reimbursement system. Furthermore, growing focus on value-based reimbursement is also fueling the growth of this market. In value-based reimbursement, quality of care and patient satisfaction are equally prioritized along with cost containment. This is encouraging more adoption of advanced healthcare reimbursement solution.
Healthcare Reimbursement Market Report Coverage
| Report Coverage | Details |
| Market Revenue in 2024 | $23.11 billion |
| Estimated Value by 2031 | $71.10 billion |
| Growth Rate | Poised to grow at a CAGR of 17.4% |
| Historical Data | 2019–2023 |
| Forecast Period | 2024–2031 |
| Forecast Units | Value (USD Million/Billion) |
| Report Coverage | Revenue Forecast, Competitive Landscape, Growth Factors, and Trends |
| Segments Covered | By Claim, By Payer, By Service Provider |
| Geographies Covered | North America, Europe, Asia Pacific, and Rest of World |
| Growth Drivers | • Growing adoption of digital reimbursement solutions • Increasing focus on value-based payment models |
| Restraints & Challenges | • Lack of healthcare infrastructure and resources • Complex reimbursement process |
Market Trends:
Cloud-based reimbursement solutions is gaining significant traction in the market. Major healthcare providers and insurers are focusing on implementing cloud-based solutions to optimize their reimbursement operations. Cloud-based solutions offer various benefits such as easy deployment, reduced operational costs, enhanced collaboration, improved scalability, and data security. For instance, Experian Health acquired Arcadia to strengthen its cloud-based population health management platform. Moreover, growing trend of automated and integrated healthcare reimbursement systems is also observed in the market. Vendors are integrating AI, machine learning and predictive analytics in their reimbursement solutions to automate the lengthy and complicated reimbursement process. This is helping to reduce paperwork and streamline reimbursement workflows.
Immediate Delivery Available | Buy This Premium Research Report: https://www.coherentmarketinsights.com/insight/buy-now/7108
Market Opportunities:
The rise of self-pay patients and increasing healthcare costs have created an opportunity for the insurance model in the healthcare reimbursement market. Under the insurance model, individuals pay a monthly or annual premium to an insurer in exchange for coverage of healthcare services. This helps provide financial protection against unexpected medical bills and ensures access to care. It accounted for around 60% market share in 2024. However, growing preference for more affordable payment options and lack of flexibility have left room for new insurance product innovations focused on tailoring coverage and easy claim settlement.
The subscription model allows individuals to pay a fixed monthly fee which grants them access to a wide range of healthcare services from primary care visits to specialist consultations to lab tests and more. It provides simplicity and predictable costs without complex plan designs or deductibles. This model captured 15% of the healthcare reimbursement market in 2024 owing to benefits like convenience, lower upfront costs and more transparency. However, limited coverage for serious medical issues and unpredictability of future needs present challenges. Innovation in supplemented high deductible plans and customized subscription tiers based on healthcare needs can boost growth.
Key Market Takeaways:
The global healthcare reimbursement market is anticipated to witness a CAGR of 17.4% during the forecast period 2024-2031, owing to increasing insurance coverage and demand for affordable healthcare plans.
On the basis of claim, the fully paid segment is expected to hold a dominant position, accounting for over 50% of the market share due to greater insurance penetration for non-catastrophic medical expenditures.
On the basis of payers, the private payers segment is expected to hold the largest share over the forecast period, due to the large number of privately purchased commercial health plans.
On the basis of service provider, the hospitals segment holds the highest share and is expected to grow at a high rate due to rising healthcare costs and inpatient volume.
Regionally, North America is expected to hold a dominant position over the forecast period, due to high medical costs and favorable regulatory environment for healthcare payers and providers.
Key players operating in the healthcare reimbursement market include UnitedHealth Group, Aviva, Allianz, CVS Health and Humana. These players are focusing on mergers, partnerships and product innovation to increase market share.
Request For Customization: https://www.coherentmarketinsights.com/insight/request-customization/7108
Recent Developments:
In April 2024, Anthem Inc. introduced a new reimbursement model for mental health services. This model includes increased reimbursement rates for mental health providers and covers a wider range of services, including digital mental health platforms. This move underscores the growing recognition of mental health as a critical component of overall healthcare.
In February 2024, UnitedHealth Group launched a new value-based care initiative designed to tie reimbursement more closely to patient outcomes rather than services provided. This initiative aims to enhance the quality of care while reducing overall healthcare costs, aligning with the broader industry shift towards value-based healthcare.
Detailed Segmentation-
By Claim:
- Fully paid
- Underpaid
By Payer:
- Private Payers
- Public Payers
By Service Provider:
- Physician office
- Hospitals & Clinics
- Diagnostic Laboratories
- Medical Equipment & Supplies
- Others
By Region:
North America:
- U.S.
- Canada
Latin America:
- Brazil
- Argentina
- Mexico
- Rest of Latin America
Europe:
- Germany
- U.K.
- Spain
- France
- Italy
- Russia
- Rest of Europe
Asia Pacific:
- China
- India
- Japan
- Australia
- South Korea
- ASEAN
- Rest of Asia Pacific
Middle East:
- GCC Countries
- Israel
- Rest of Middle East
Africa:
- South Africa
- North Africa
- Central Africa
Browse Related Reports:
Face Recognition Ai Camera Market: Global face recognition AI camera market is estimated to be valued at USD 3.08 Bn in 2024 and is expected to reach USD 12.71 Bn by 2031, exhibiting a compound annual growth rate (CAGR) of 22.4% from 2024 to 2031.
Accountable Care Solutions Market: Global accountable care solutions market is estimated to be valued at US$ 21.50 Bn in 2024 and is expected to reach US$ 42.54 Bn by 2031, exhibiting a compound annual growth rate (CAGR) of 10.2% from 2024 to 2031.
B2B Payments Transaction Market: The B2B payments transaction market is estimated to be valued at US$ 1,576.61 Bn in 2024 and is expected to reach US$ 3,021.25 Bn by 2031, growing at a compound annual growth rate (CAGR) of 9.7% from 2024 to 2031.
Agricultural Drones Market: Global agricultural drones market is estimated to be valued at US$ 4.80 Bn in 2024 and is expected to reach US$ 19.24 Bn by 2031, exhibiting a compound annual growth rate (CAGR) of 21.9% from 2024 to 2031.
Author Bio:
Ravina Pandya, PR Writer, has a strong foothold in the market research industry. She specializes in writing well-researched articles from different industries, including food and beverages, information and technology, healthcare, chemical and materials, etc. With an MBA in E-commerce, she has an expertise in SEO-optimized content that resonates with industry professionals. (LinkedIn: https://www.linkedin.com/in/ravina-pandya-1a3984191)
About Us:
Coherent Market Insights is a global market intelligence and consulting organization that provides syndicated research reports, customized research reports, and consulting services. We are known for our actionable insights and authentic reports in various domains including aerospace and defense, agriculture, food and beverages, automotive, chemicals and materials, and virtually all domains and an exhaustive list of sub-domains under the sun. We create value for clients through our highly reliable and accurate reports. We are also committed in playing a leading role in offering insights in various sectors post-COVID-19 and continue to deliver measurable, sustainable results for our clients.
